The HLA-A Gene
The human leukocyte antigen (HLA) system is a critical component of the immune system and an essential subject of medical research. The major histocompatibility complex (MHC) is an integral part of the HLA system, and the HLA-A gene is a key gene within this complex. This gene plays an important role in the body’s ability to recognize and respond to foreign pathogens, making it a crucial research topic in the field of immunology. This article will discuss the significance of the HLA-A gene in medical research, exploring its role in the body’s immune system and its potential applications in the development of treatments and therapies.
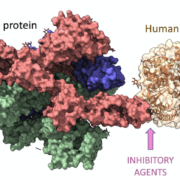
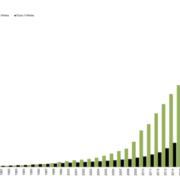
The HLA-A gene is a part of the human leukocyte antigen (HLA) complex and is located on the short arm of chromosome 6 (6p21.3). It encodes for a family of proteins that are major histocompatibility complex (MHC) class I molecules. The MHC class I molecules are involved in the recognition and presentation of peptide antigens to the immune system’s T cells, which are key players in the body’s adaptive immune system. HLA-A is the most polymorphic gene in the human genome, meaning that it has the highest number of different variants, and is thus highly variable between individuals. This variability is important for the immune system, as it allows the body to recognize a wide range of foreign antigens and mount an appropriate immune response.
Research on the HLA-A gene has had a major impact on the medical field, particularly in the areas of transplantation, autoimmune diseases, and cancer. HLA-A is an important gene in the major histocompatibility complex (MHC), which is responsible for regulating the immune system.
In transplantation, research on HLA-A has enabled clinicians to better match donors and recipients to reduce the risk of organ rejection. By identifying the specific HLA-A antigens of the donor and the recipient, clinicians can determine which organs are the best genetic match. This has enabled more successful transplantations, with fewer complications.
In autoimmune diseases, research on HLA-A has helped to identify which genetic variants are associated with different diseases, such as type 1 diabetes, rheumatoid arthritis, and inflammatory bowel disease. By understanding the genetic basis of these diseases, clinicians can develop more targeted therapies that are tailored to the individual patient.
Finally, in cancer, research on HLA-A has helped to identify which patients are at an increased risk of certain types of cancer, such as melanoma. By identifying individuals with particular HLA-A variants, clinicians can develop more effective screening and prevention strategies.
Variations or mutations in any part of the HLA-A gene can have various effects on a person’s health and immunity, depending upon which specific amino acid sequence has been altered by mutation. Some common examples include: weakened immune responses, increased risk for autoimmune diseases such as type 1 diabetes mellitus or Grave’s disease, delayed allergic reactions to drugs or other substances due to decreased recognition of foreign molecules by T cells; increased susceptibility to infectious diseases caused by viruses like HIV/AIDS; decreased production of cytokines needed for inflammation; malignant transformation into cancerous tumors; reduction in NK cell activity leading to a greater chance for tumor development.
Research has shown that specific variants of the HLA-A gene can influence a person’s risk for developing autoimmune disorders such as type 1 diabetes, rheumatoid arthritis, and systemic lupus erythematosus. For example, two common alleles (variants) of HLA-A known as *03:01* and *02:01* have been linked to increased risk for type 1 diabetes, while another allele (*04:05*) appears to protect against it. Additionally, research suggests that some HLA-A alleles can increase or decrease the risk for celiac disease depending on what other related genes they interact with. Furthermore, several studies have identified associations between particular versions of this gene and HIV infection outcomes—for example, one study suggested that individuals carrying certain alleles had better treatment outcomes than those lacking them. Finally, recent evidence indicates there may be links between certain HLA-A variants and altered levels of cytokines responsible for inflammation in people with psoriasis vulgaris—a chronic skin condition characterized by red scaly patches often present on elbows knees scalp face palms soles etc.
Continued research on the HLA-A gene is essential to ensure that we are able to unlock its full potential for human health. As this gene has been associated with numerous diseases, understanding its underlying genetic mechanisms could lead to new and improved treatments or even cures. Additionally, by learning more about this gene’s role in disease susceptibility, we can develop better preventive strategies against these conditions. Ultimately, researching the HLA-A gene provides us with a powerful opportunity to improve public health on a global scale.



 The Sequencing Center
The Sequencing Center

Leave a Reply
Want to join the discussion?Feel free to contribute!